How Do Biotech Startups Use a QMS to Support Clinical Trial Readiness?

Biotech startups operate at the intersection of speed and scrutiny. While teams are under pressure to advance science, secure funding, and move programs into the clinic, regulators expect discipline, documentation, and control from day one of clinical development. Clinical trial readiness is not achieved through last-minute preparation. It is built through systems that ensure consistency, traceability, and accountability over time. A Quality Management System (QMS) provides the structure biotech startups need to meet these expectations without slowing progress.
For startups entering or operating within clinical trials, a QMS functions as the backbone of compliance and operational oversight. It allows organizations to demonstrate that work is performed under control, decisions are documented and justified, and quality issues are managed systematically. Rather than relying on informal processes or individual knowledge, startups use a QMS to embed quality into daily clinical operations.
What Clinical Trial Readiness Means for Biotech Startups
Clinical trial readiness means being able to show regulators, sponsors, and partners that the organization maintains control over its clinical activities at all times. This includes demonstrating that procedures are defined and followed, personnel are trained and qualified, data integrity is protected, and risks are actively managed. Readiness is not tied to a single inspection or milestone. It reflects an ongoing state in which the organization can respond to questions with evidence, not assumptions.
For biotech startups, readiness is especially important because resources are limited and many activities are outsourced. Regulators recognize this reality, but they still expect sponsors to retain oversight and accountability. A QMS provides the framework that allows startups to meet these expectations in a consistent and defensible way.
The Role of QMS in Sponsor Oversight
In most biotech startups, clinical trials are executed through a network of CROs, laboratories, manufacturers, and specialized vendors. While these partners perform critical work, responsibility for quality and compliance always remains with the sponsor. A QMS defines how that responsibility is exercised.
Through documented procedures, oversight plans, and quality records, the QMS establishes how vendors are selected, qualified, monitored, and evaluated. It captures how decisions are made, how issues are escalated, and how corrective actions are implemented. This allows startups to demonstrate that outsourcing does not mean relinquishing control. Instead, the QMS shows that vendor activities are governed within a structured quality framework.
Document Control as the Foundation of Trial Readiness
Document control is often the first capability biotech startups implement within a QMS. Clinical development relies on controlled documentation, including SOPs, quality plans, oversight procedures, and records that support trial conduct. Without formal control, documents quickly become outdated, inconsistent, or misapplied.
A QMS centralizes document management and enforces version control, approval workflows, and effective dates. It ensures that only approved procedures are in use and that historical versions remain available for reference. When regulators ask which procedure governed an activity at a specific point in time, the QMS provides a clear and traceable answer. This level of control reduces risk and builds confidence in the organization’s clinical operations.
Training Management and Role Qualification
Training is a frequent focus during clinical inspections. Regulators expect sponsors to demonstrate that personnel performing clinical and quality-related activities are qualified for their roles. This expectation extends beyond internal staff to individuals responsible for vendor oversight and quality decision-making.
A QMS connects training requirements directly to roles and procedures. When a procedure is updated, the system triggers retraining for impacted personnel. Training records are maintained in a controlled and auditable format, allowing startups to show that staff were trained on the correct version of procedures at the appropriate time. This approach replaces informal or ad hoc training practices with a system that supports compliance and inspection readiness.
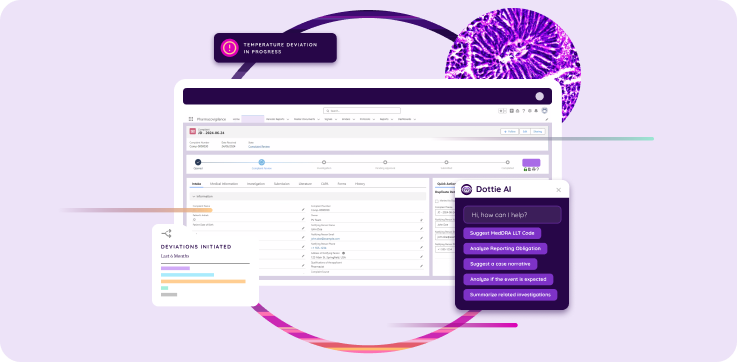
Managing Deviations and Quality Events
Deviations and quality events are inevitable during clinical trials. These may include protocol deviations, data discrepancies, vendor errors, or process breakdowns. The difference between a mature organization and an unprepared one lies in how these issues are handled.
A QMS provides a standardized way to capture, assess, and manage quality events. Each event is documented, assigned an owner, evaluated for impact, and tracked through resolution. This consistency ensures that issues are addressed systematically rather than reactively. It also allows startups to demonstrate control over trial conduct and transparency in how problems are identified and resolved.
CAPA as a Measure of Organizational Maturity
Corrective and Preventive Action (CAPA) is one of the most scrutinized aspects of a quality system. Regulators expect sponsors to identify root causes, implement appropriate actions, and verify that those actions prevent recurrence. A QMS enforces this discipline.
When a deviation or audit finding triggers CAPA, the QMS guides the organization through structured investigation, action planning, and effectiveness checks. CAPA records remain linked to the originating issue, providing full traceability. This demonstrates that the startup learns from problems and strengthens its system over time, an important signal of quality maturity even in early-stage organizations.
Change Control in a Dynamic Clinical Environment
Clinical development is characterized by constant change. Protocol amendments, vendor transitions, system updates, and procedural revisions are common. Regulators expect these changes to be managed in a controlled and documented manner.
A QMS provides a framework for change control that ensures changes are reviewed for impact before implementation. It captures the rationale for change, assesses potential effects on patient safety, data integrity, and compliance, and routes approvals to the appropriate stakeholders. Training and documentation updates are automatically linked, ensuring changes are implemented consistently across the organization. This prevents undocumented or poorly assessed changes that can undermine trial integrity.
Vendor Qualification and Ongoing Oversight
Because biotech startups rely heavily on external partners, vendor oversight is a critical component of clinical trial readiness. A QMS supports vendor qualification by documenting due diligence activities, defining responsibilities through quality agreements, and tracking performance over time.
Ongoing oversight activities, including audits, performance reviews, and issue management, are captured within the QMS. This provides clear evidence that the sponsor actively monitors vendor quality and responds to issues appropriately. When inspectors ask how vendor compliance is ensured, the QMS offers a complete and traceable record.
Protecting Data Integrity Through QMS Governance
Data integrity is central to clinical trial credibility. Regulators expect sponsors to protect data from creation through reporting and archiving. A QMS supports data integrity by defining access controls, audit trail review practices, and record retention requirements.
The QMS also governs how computerized systems used in clinical trials are validated and maintained. By documenting system inventories, validation approaches, and change management processes, startups can demonstrate that their digital tools are fit for purpose and used as intended. This is especially important as clinical trials become increasingly data-driven and technology-enabled.
Risk Management Aligned With Trial Execution
Modern regulatory expectations emphasize risk-based quality management. A QMS allows startups to document how risks are identified, assessed, and mitigated throughout the clinical trial lifecycle. Risks related to protocol execution, vendors, data quality, and patient safety can be tracked and reviewed as trials progress.
By linking risk management to quality events, monitoring strategies, and CAPA, the QMS ensures that risk management remains active rather than static. This alignment strengthens oversight and demonstrates a thoughtful approach to trial execution.
Scaling QMS Without Slowing Development
Biotech startups typically implement their QMS in phases. Early efforts focus on essential controls such as document management, training, deviations, CAPA, and change control. As trials advance and organizational complexity increases, additional capabilities are added. This phased approach allows startups to build quality maturity while maintaining operational agility.
Building Continuous Inspection Readiness
True inspection readiness is embedded in daily operations. A QMS enables startups to retrieve records, training evidence, and decision histories quickly and confidently. Rather than preparing for inspections as isolated events, teams operate in a state of continuous readiness. This reduces stress, shortens response times, and builds trust with regulators and partners.
Why QMS Is a Strategic Asset for Biotech Startups
A QMS does more than support compliance. It provides clarity, consistency, and control as biotech startups transition from research to clinical development. By embedding quality into daily work, startups reduce rework, prevent repeated issues, and support informed decision-making.
For biotech startups preparing for or conducting clinical trials, a QMS is not an administrative burden. It is a strategic system that enables trial readiness, regulatory confidence, and sustainable growth.